This website uses cookies to help us give you the best experience when you visit and for certain analytics and marketing activities. By continuing to use this website, you consent to the use of these cookies. Please exit the website if you do not agree to such cookies being used. To find out more about how we use cookies, go to our Privacy Policy.
Newborns to Adults 18+
Screening and monitoring of patients

Newborn Screening
Galactosemia screening methods for newborns
Classic Galactosemia is suspected in individuals with the following newborn screening results, clinical features, family history, and supportive laboratory findings1:
Newborn screening utilizes a small amount of blood obtained from a heel prick to quantify2:
- Total content of erythrocyte galactose-1-phosphate and blood galactose concentration1
- Erythrocyte GALT enzyme activity1
- Biallelic pathogenic variants in GALT1
State Newborn Screening (NBS) programs vary as to which of these tests is performed and in what sequence.1

Diagnostic Testing
Analyzing Gal-1p and GALT
Diagnostic testing to detect Classic Galactosemia could involve1:
- Detection of elevated erythrocyte Gal-1p concentration
- Reduced erythrocyte GALT enzyme activity
- Biallelic pathogenic variants in GALT
Early reactions in Galactosemia
Monitoring methods for newborns
A newborn with Classic Galactosemia experiences life-threatening complications within days after ingesting breast milk or a lactose-containing formula. Without dietary galactose restriction, manifestations of Galactosemia include: feeding problems, failure to thrive, liver damage, lethargy, seizures, and sepsis (mostly E. coli).1,3
RESEARCH
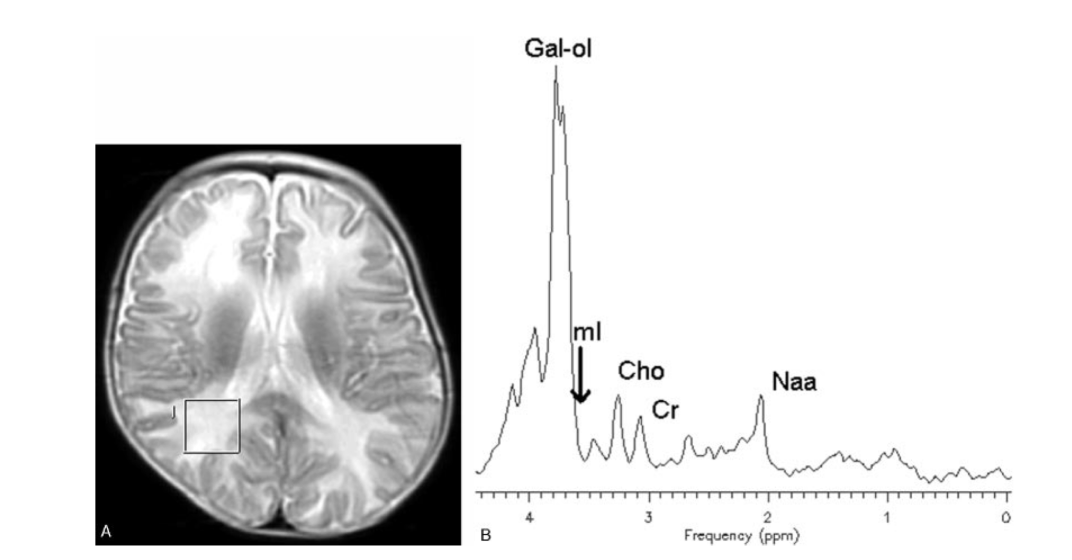
MRS imaging demonstrates high levels of toxic galactitol in the brain4
Infants with Galactosemia who continue to consume galactose reveal extremely high levels of toxic galactitol in their brains as demonstrated by magnetic resonance spectroscopy (MRS) images.4,5
With dietary restriction of galactose, early acute complications usually self-resolve and liver failure, sepsis, and death are typically avoided. However, while some abnormalities observed with MRS images self-resolve, other abnormalities in cognitive and language centers in the brain persist and are associated with long-term developmental complications.1,3
Endogenous galactose is never eliminated via diet management and as the child develops, the prevalence of galactose in virtually all foods makes complete elimination of dietary galactose nearly impossible.3,6,7
MRS Example. See: Otaduy et al. AJNR Am J Neuroradiol. 2006; 27:204-207.
With dietary restriction of galactose, early acute complications usually self-resolve and liver failure, sepsis, and death are typically avoided. However, while some abnormalities observed with MRS images self-resolve, other abnormalities in cognitive and language centers in the brain persist and are associated with long-term developmental complications.1,3
Endogenous galactose is never eliminated via diet management and as the child develops, the prevalence of galactose in virtually all foods makes complete elimination of dietary galactose nearly impossible.3,6,7
Monitoring at Every Life Stage
How to monitor for developmental delays
To monitor developmental delays, international guidelines for the management of Classic Galactosemia recommend age-appropriate testing for cognitive development and status. Testing includes assessments of, but are not limited to, the following3:
After the age of 15, continued assessment should be based on individual patient needs. View detailed assessment guidelines.
Neurological defects persist and/or worsen throughout adulthood
Studies in adolescents and young adults with Galactosemia have shown both white and grey matter abnormalities consistent with the cognitive impairment, language problems, and motor disturbances observed beginning in early childhood.4,5
Galactitol production also contributes to ovarian dysfunction. Nearly all females with Classic Galactosemia develop primary ovarian insufficiency. Although the exact mechanism of ovarian dysfunction has not been identified, both direct deposition of galactitol and oxidative stress induced by galactitol production are believed to contribute to this problem.8-11
Neurological deficits may diminish adult quality of life10,12
In adults, CNS deficits contribute to:
- Lower academic attainment
- Less skilled employment, more unemployment
- An inability to form social bonds, including marriage
- An inability to maintain independence (living with parents)
Looking Ahead
Long-term complications and patient surveillance
Patients with Galactosemia may exhibit extreme heterogeneity in the complications that manifest over time. Clinical findings in early disease do not predict long-term outcomes. Moreover, there is little or no correlation between the time when dietary restriction is initiated and developmental delays, and associations of specific complications with genotype remain unclear. Therefore, vigilant surveillance of patient health status is essential.1,3
In adolescents with Galactosemia
Approximately one-half of patients with Classic Galactosemia experience developmental delays that emerge in infancy or early childhood and then progress.
In what percentage of adolescents with Galactosemia do these symptoms occur?13
Motor function
Cognition
Language
References
- Berry GT. Classic galactosemia and clinical variant galactosemia. In: Adam MP, Ardinger HH, Pagon RA, et al, eds. GeneReviews®. Seattle (WA): University of Washington; February 4, 2000.
- Baby's First Test. Newborn Screening 101. Updated October, 2018. Accessed October 12, 2020. https://www.babysfirsttest.org/newborn-screening/screening-101
- Welling L, Bernstein LE, Berry GT, et al. International clinical guideline for the management of classical galactosemia: diagnosis, treatment, and follow-up. J Inherit Metab Dis. 2017;40(2):171-176. doi:10.1007/s10545-016-9990-5
- Otaduy MCG, Leite CG, Lacerda MTC, et al. Proton MR spectroscopy and imaging of a galactosemic patient before and after dietary treatment. AJNR. 2006;27:1-4.
- Berry GT, et al. In vivo evidence of brain galactitol accumulation in an infant with Galactosemia and encephalopathy. J Ped. 2001;138(2):260-262.
- Schadewaldt P, et al. Age dependence of endogenous galactose formation in Q188R homozygous galactosemic patients. Mol Gen and Metab. 2004;(81):31-44.
- Bosch AM. Classic galactosemia: dietary dilemmas. J Inherit Metab Dis. 2011;34:257-260.
- Fridovich-Keil JL, Gubbels CS, Spencer JB, Sanders RD, et al. Ovarian function in girls and women with GALT-deficiency galactosemia. J Inherit Metab Dis. 2011;34:357-366.
- Fridovich-Keil J, Bean L, He M, et al. Epimerase deficiency galactosemia. 2011 [Updated 2016 Jun 16]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews®. Seattle (WA): University of Washington, Seattle; 1993-2020.
- Coelho AI, Rubio-Gozalbo ME, Vicente JB, Rivera I. Sweet and sour: an update on classic galactosemia. J Inherit Metab Dis. 2017;40:325-342. doi:10.1007/s10545-017-0029-3
- Forges T, et al. Pathophysiology of impaired ovarian function in galactosemia. Human Reprod. 2006;12(5):573-584.
- Waisbren SE, Potter NL, Gordon CM, et al. The adult galactosemic phenotype. J Inherit Metab Dis. 2012;35(2):279-286. doi:10.1007/s10545-011-9372-y
- Rubio-Gozalbo ME, Haskovic M, Bosch AM, et al. The natural history of classic galactosemia: lessons from the GalNet registry. Orphanet J Rare Dis. 2019;14(1):86. doi:10.1186/s13023-019-1047-z

